BASAL CELL CARCINOMA
Basal cell carcinoma is the most common type of skin cancer that dermatologists detect and diagnose in the United States each year. In fact, basal cell carcinoma is the most frequently occurring form of all cancers.
What Is Basal Cell Carcinoma?
Basal cell carcinomas develop from the basal cells of the epidermis (the outermost layer of skin). In normal skin, the basal cells are responsible for producing new skin cells as old skin cells are shed off. Basal cell carcinoma occurs when UV radiation from the sun or tanning beds damages the basal cells leading to uncontrolled growth and proliferation.
Because the damage to the basal cells is caused by UV radiation, basal cell carcinomas typically develop on areas of your body that get chronic exposure to the sun, such as the head and neck. UV radiation from indoor tanning beds can also damage the basal cells leading to an increased risk for skin cancers.
What Are the Symptoms of Basal Cell Carcinoma?
Knowing the signs and symptoms of a basal cell carcinoma can help with the early detection and treatment.
What can a basal cell carcinoma look like?
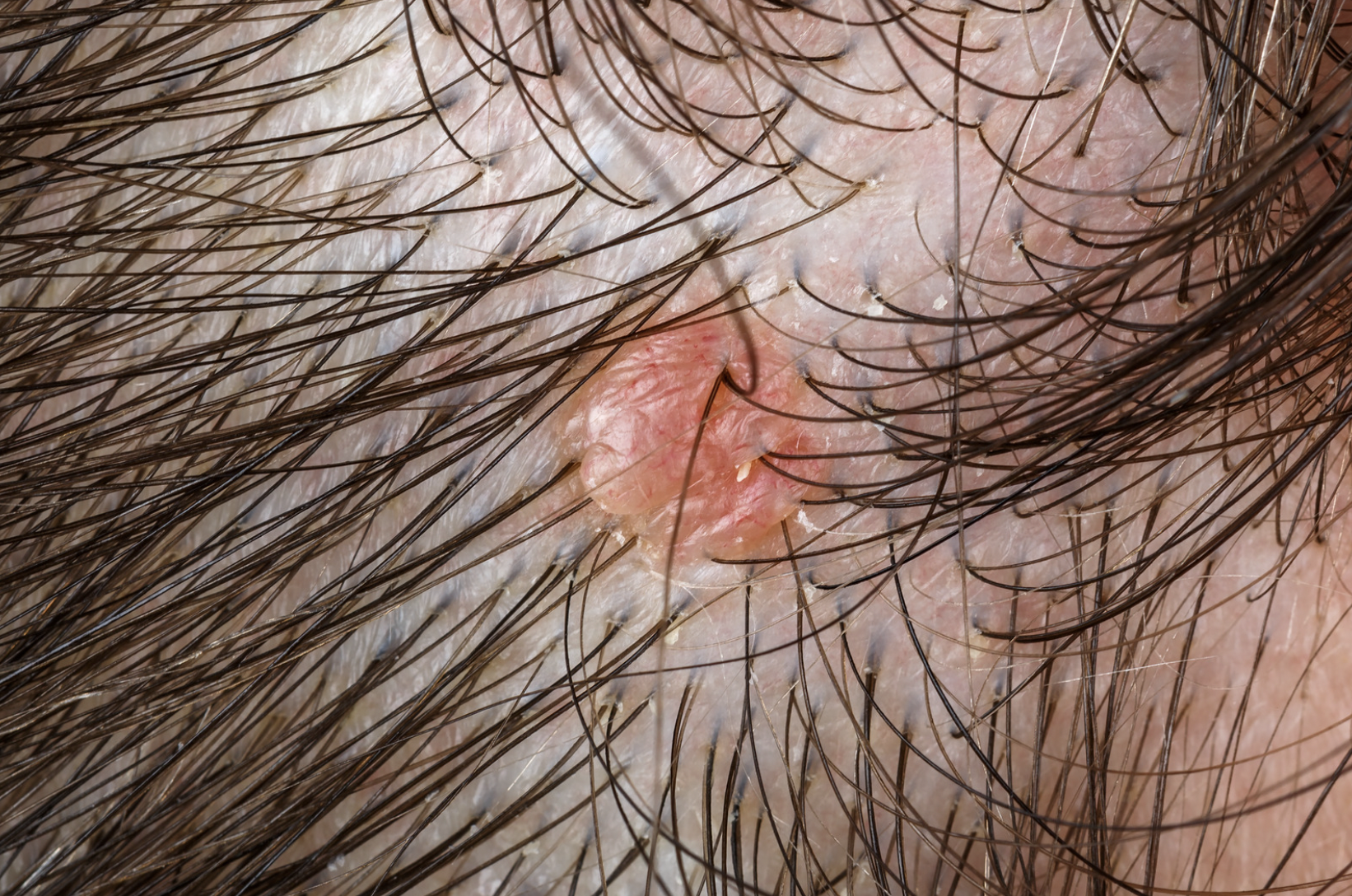
- An open sore that does not heal
- A shiny or “pearly” bump which can be flesh colored, pink, or even speckled with brown or black pigment
- A pink and/or scaly growth
- A white, waxy, scar-like area
- A growth with rolled borders and a central crust or ulcer

What Are the Risk Factors for Basal Cell Carcinoma?
Common risk factors for developing basal cell carcinomas include:
- UV radiation in the form of sun exposure or use of tanning beds
- Fair skin
- Increasing age
- Male sex
- A personal or family history of skin cancer
- Weakened immune system because of illness or certain immune-suppressing drugs such as those taken by transplant patients
Protecting your skin from the sun can help reduce your risk for basal cell carcinomas. Dermatologists recommend avoiding the sun during its peak hours, applying broad-spectrum sunscreen (SPF 30 or higher), and wearing sun-protective clothing. The use of tanning beds is also strongly discouraged.
How Is Basal Cell Carcinoma Diagnosed
Any new, unusual, changing, or symptomatic growth should prompt a visit to your dermatologist. If you have risk factors (personal or family history of skin cancers, transplant recipient, significant sun exposure or tanning bed use in the past, etc), scheduling regular appointments with your dermatologist can help with accurate and timely diagnosis and treatment of skin cancers.
At your visit, your dermatologist will evaluate your skin and any lesions or growths of concern. A skin biopsy (a procedure that removes a small sample of the skin) is usually done to confirm a definitive diagnosis. Once the diagnosis of squamous cell carcinoma has been confirmed, your dermatologist will discuss treatment options.
Treatment for Basal Cell Carcinoma
When detected early, most basal cell carcinomas can be easily treated and cured. Treatment is important because basal cell carcinomas will continue to grow and spread if left untreated. While basal cell carcinomas rarely metastasize (spread beyond the original skin cancer site), basal cell carcinomas can grow larger and deeper, destroying the local skin and tissue and causing non-healing sores and disfigurement.
The most common treatment options for basal cell carcinomas include:
Curettage and Electrodessication (ED&C)
Curettage and electrodessication are commonly used to treat small, well defined basal cell carcinomas. During the procedure, a dermatologist uses a sharp round instrument called a curette to scrape away at the skin cancer cells. After scraping the site, heat is then applied to destroy the remaining skin cancer cells and control the bleeding. The scraping and heat application may be repeated a few times during the treatment session to ensure the removal of the basal cell carcinoma. The procedure usually leaves behind a round white scar.
Excision
Surgical excision is commonly used to remove basal cell carcinomas. During the procedure, the dermatologist uses a blade called a scalpel to excise or cut out the skin cancer. The visible skin cancer along with a margin of normal skin at the skin cancer border is removed and sent off for evaluation at a pathology lab to ensure that the skin cancer was completely removed. The surgical site is then closed with sutures. The procedure usually leaves behind a line or linear scar.
Mohs Surgery
Mohs surgery is a specialized technique used to treat skin cancers in sensitive locations such as the eyes, nose, lips, ears, fingers, and toes. It is also the treatment of choice for large and/or aggressive skin cancers with poorly defined borders.
During the procedure, a Mohs surgeon will remove the visible skin tumor along with a very small margin of normal skin at the skin cancer border. While the patient is still present in the office, the tissue is processed and evaluated by the Mohs surgeon to determine if any skin cancer cells persist and where the persistent skin cancer cells reside. If skin cancer cells are still present, the Mohs surgeon will return to the patient to remove additional tissue at the exact site where skin cancer cells were noted. The process is repeated in stages, each time removing additional tissue and checking for residual skin cancer, until there is no evidence of any remaining skin cancer.
Mohs surgery ensures that the skin cancer has been completely removed while preserving as much normal skin as possible.
Radiation Therapy for Basal Cell Carcinoma
Radiation therapy is primarily used as a second line therapy in patients who are not good candidates for surgery. For advanced or aggressive basal cell carcinomas, radiation therapy can also be used in combination with surgery.
During radiation therapy, low-energy x-ray beams are used to destroy the skin cancer cells. Treatment of the skin cancer requires numerous treatments over a period of time, usually weeks to months.
Cryosurgery
Thin, superficial, early basal cell carcinomas can be treated with cryotherapy. Liquid nitrogen is applied to the basal cell carcinoma which freezes and destroys the skin cancer cells.
Photodynamic therapy (PDT)
Thin, superficial, early basal cell carcinomas can also be treated with photodynamic therapy. During the procedure, a light sensitizing topical agent is applied to the affected areas. Following a period of time for absorption, the treated area is then exposed to a light or laser, generating a reaction that destroys the skin cancer cells.
Using Topical Therapies for Basal Cell Carcinoma
5-fluorouracil (5-FU, Efudex, Carac, Fluoroplex, Tolak) and imiquimod (Aldara, Zyclara) are topical preparations that can be applied directly to the skin to treat superficial, thin basal cell carcinomas.
5-fluorouracil is a chemotherapy cream that selectively targets and destroys the actively dividing cells of skin cancers. Imiquimod activates the immune system to destroy the skin cancer cells.
Treating your skin cancer with a topical preparation requires diligent use of the cream to the affected area for the prescribed amount of time. Frequently, it requires applying the medication once or twice daily for a period of weeks. If selected as your method of treatment for your basal cell carcinoma, your dermatologist will provide detailed instructions on how often and how long to use the topical.
During treatment, expect the site to become red, scaly, and inflamed as the medication eradicates the skin cancer cells.
Contact Dermatology & Surgery Associates to learn more about squamous cell carcinoma.
Thousands of Bronxites Trust Dermatology and Surgery Associates
Dermatology & Plastic Surgery Under One Roof
Learn More About Our
Dermatology Services
Learn More About Our
Plastic Surgery Services
Dermatology and Surgery Associates | 3620 E Tremont Ave NY 10465 | 718.568.6401 | Pay Online | Patient Forms
By Dermatology and Surgery Associates | © 2022 All Rights Reserved. Design & Development by Goldman Marketing Group | Sitemap | Privacy Policy | The information available on this web site is provided for informational purposes only. This information is not intended to replace a medical consultation where a physician’s judgment may advise you about specific disorders, conditions and or treatment options. We hope the information will be useful for you to become more educated about your health care decisions. If you are vision-impaired or have some other impairment covered by the Americans with Disabilities Act or a similar law, and you wish to discuss potential accommodations related to using this website, please contact us at 201.584.5253.

